
News
Dental clinicians can help to improve dentine hypersensitivity and quality of life for their patients significantly – but for treatment to be successful, it has to be a joint effort.
This was the shared opinion of three leading dental clinicians speaking at the BioMin expert panel session held as part of the Online Dentistry Show on 19 March. In a hugely creative response to the coronavirus pandemic, the Online Dentistry Show brought together manufacturers and clinicians online, offering a range of talks, demonstrations and industry stands, mimicking a real dental show, where dental professionals could discuss clinical and management issues.
The BioMin expert session took the form of an innovative panel-based discussion, led by presenter and dental therapist, Victoria Wilson, in conversation with Dr David Gillam, Clinical Reader in periodontology at the Barts London School of Medicine and Dentistry; private perio specialist Dr Reena Wadia; and Siobhan Kelleher, owner of Dental Hygienist.ie, an award winning dental hygiene practice in Ireland, who uses coaching techniques to effect behaviour change in patients. Each expert gave a different but complementary approach to the issue of dentine hypersensitivity (DH) and its management, with a view to reducing its impact on patients’ quality of life.
Dr David Gillam, looking at the question of diagnosis and treatment, said that many clinicians underestimated DH’s impact on quality of life and were not confident in managing it. He gave a brief recap on the role of BioMin F toothpaste as a treatment for DH, explaining how its slow release mechanism, gradually releasing an optimum balance of fluoride, phosphate and calcium ions, produced fluorapatite, effective both at reducing the symptoms of DH and remineralising lost tooth enamel.
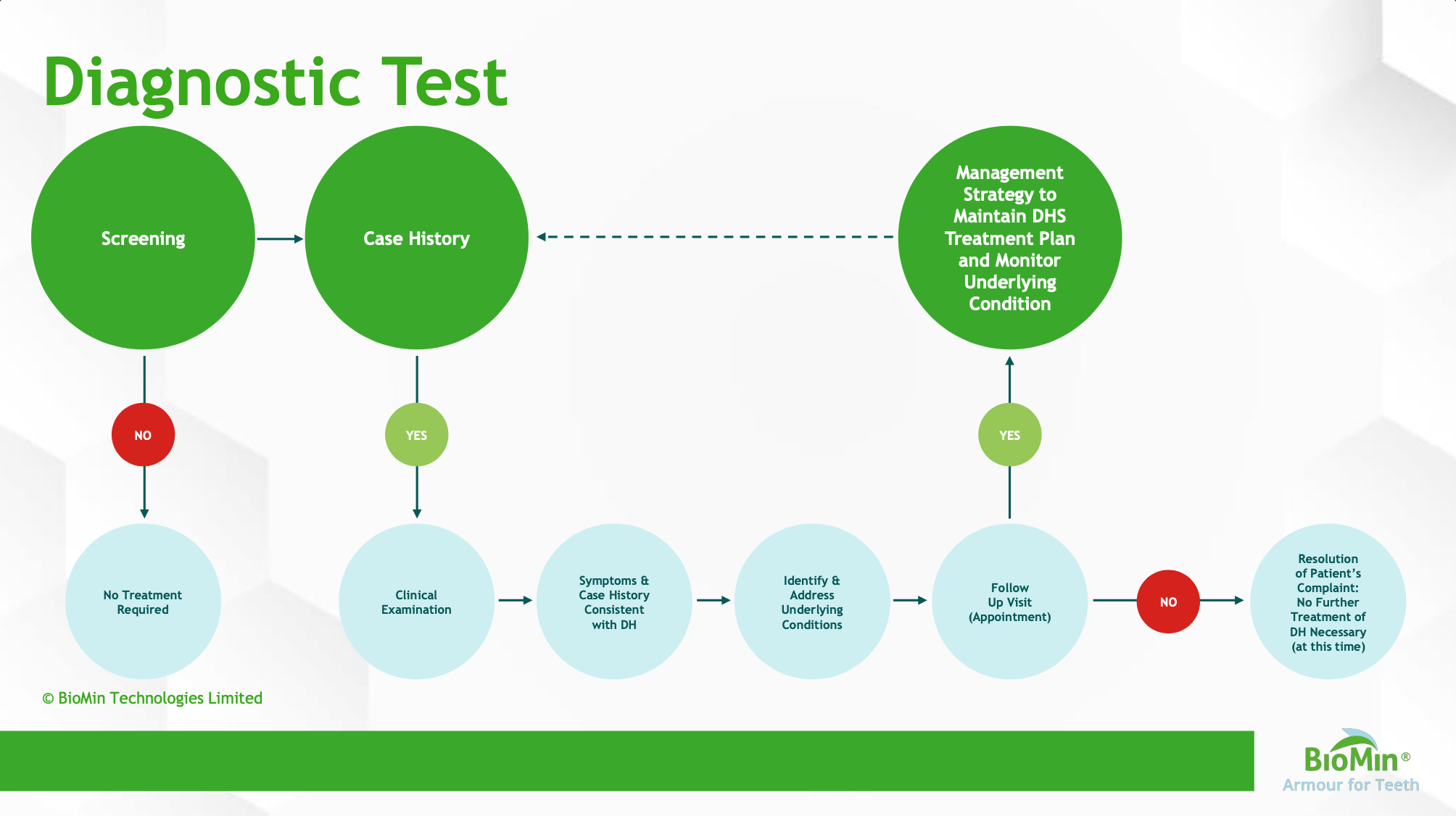
Dr Gillam outlined a simple but effective diagnostic tool for clinicians to use in their practice, and a treatment path, stepping up the level of intervention depending on the severity of the discomfort and whether or not it responded to advice about toothbrushing technique, dietary advice and the use of a desensitising toothpaste.
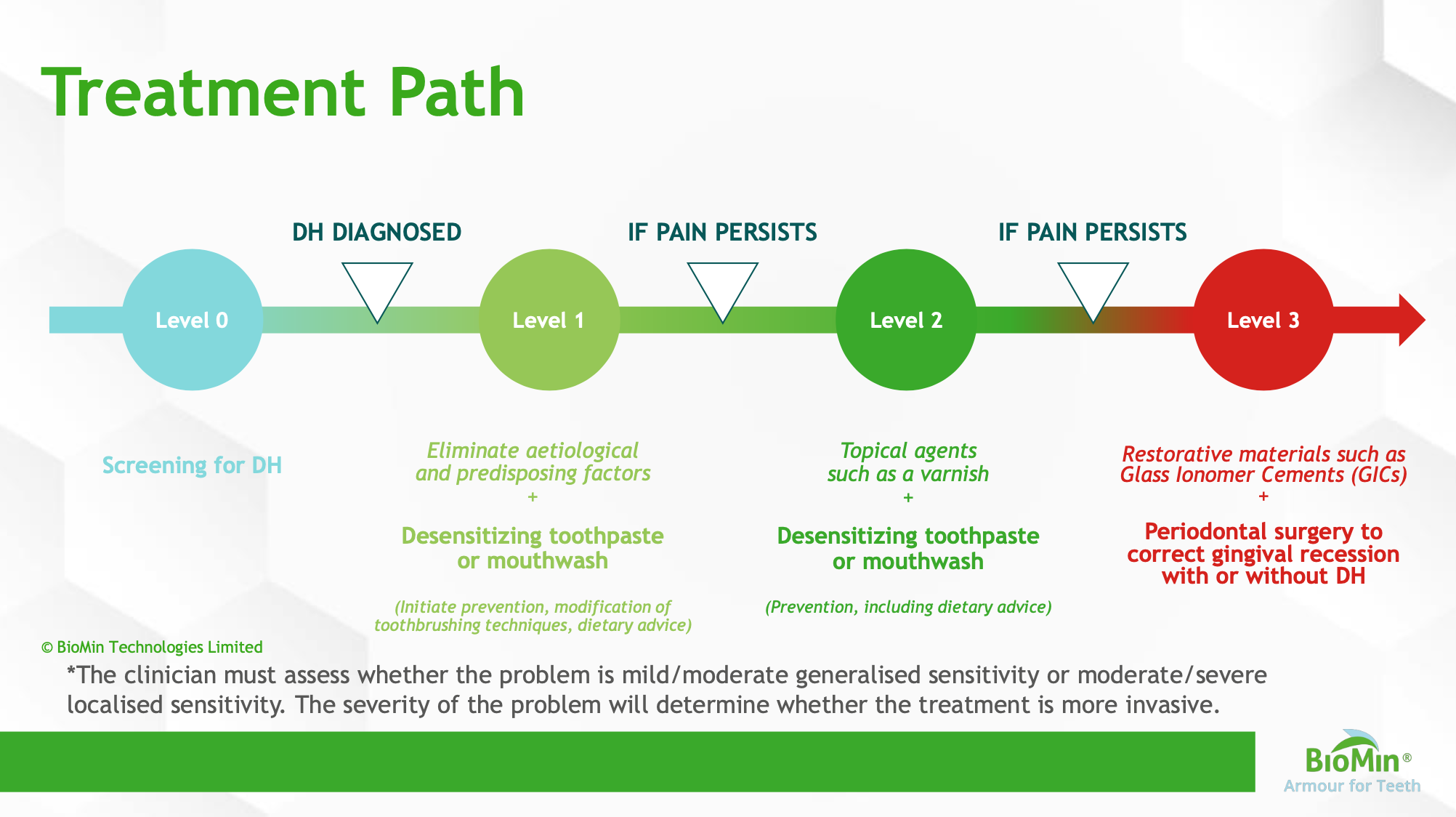
‘The clinician must assess whether the problem is mild/moderate generalised sensitivity or moderate/severe localised sensitivity,’ he said. ‘The severity of the problem will determine whether the treatment is more invasive.’
He added: ‘It’s not simply giving the treatment or procedure, it’s about giving preventive advice - altering the patient’s behaviour and modifying what they do within their day to day lifestyle.’
Dr Gillam suggested that clinicians use the principles that he outlined, but tailor them to what was workable in their own practice. He also warned that it might not be possible to get the pain of DH down to zero, and so clinicians needed to manage both their and their patients’ expectations. ‘If we can reduce the discomfort to a level where they can cope with their day-to-day practices of rinsing, eating and so on, I think that is still a benefit,’ he said.
Dr Reena Wadia, associate specialist at King’s College Hospital as well as a Harley Street periodontist, believes that over 50% of her patients suffer from DH, with an impact on their quality of life. She stressed the importance of warning patients in advance that perio treatment can cause sensitivity. ‘This should be a key discussion point during our consent process, pre-treatment,’ she insisted. It’s also important to reassure the patient that despite this, the clinician will do their best to reduce or eliminate the symptoms.
Dr Wadia’s practice takes a team approach to this, involving the hygienists, the referring clinicians and the patient. ‘It’s a joint effort,’ she said.
‘It’s got to be 360,’ she said. ‘You’re not just treating dentine hypersensitivity. Take a thorough history and work out what might be exacerbating the DH, including if necessary involving medical management by a GP. You need to be managing it actively, including advice on homecare products, looking at it 360 but also taking a step by step approach.’
She added: ‘Patient reported outcomes in the current day and age are just as important as clinical outcomes.’ She stressed the importance of optimal homecare, ensuring the patient is using a product that is effective against sensitivity, and of giving really basic advice, like spitting not rinsing.
At the end of every treatment, regardless of whether it is treatment or maintenance, Dr Wadia and her team always apply BioMin to reduce the likelihood of sensitivity occurring – and her patients appear to prefer the melon flavour of BioMin F for Kids. ‘By applying BioMin we are occluding the tubules post treatment and we have had fantastic feedback from patients,’ she said. BioMin is also applied mid-treatment and at follow-up appointments. ‘It significantly helps with sensitivity and patients notice that you are taking the extra step to protect them.’
Patients with pre-existing sensitivity problems are the most challenging to treat, said Dr Wadia, and they are often also the most anxious after previous bad experiences. ‘Take a stepwise approach, telling them what you are doing, making them as calm as possible, showing them they can trust you, giving them a good experience so they are wanting to come back – and they are also the most satisfying to treat as well.’
‘Make sure they’re comfortable first, then find out why they are getting the sensitivity, and what you can do to help them – and explain what you are doing,’ she said. ‘We are healthcare professionals and we need to look at the patient as a whole, not just focus in on that tooth.’
Discussing the management of DH through behavioural change, hygienist and coach Siobhan Kelleher takes the approach of motivational interviewing, gathering information about the patient, engaging with them and make a plan with them.
She explained: in the RULE principle, R is for resistance, where the clinician needs to overcome that fighting reflex by allowing the patient to be the expert in their own condition, ‘co-creating the appointment together’. U is for understanding what is going on with the patient and what the patient wants out of the appointment; L for active listening, really picking up on what the patient is saying; and E for empowering, where she uses an iPad or other tools to give the patient information and help and support them.
‘Patients with DH are so grateful for any help you can offer because it really impacts on their quality of life from day to day,’ she said. She uses a 1-10 scale to grade the level of pain, with above 7 being severe, and to measure the impact on their quality of life. This is recorded in the notes so that she can refer back to it and monitor the response. She is then able to check whether she can help, for example with product recommendation, or whether she needs to bring in other people, like the dentist or a specialist, for example in occlusion.
She stressed the importance of review – following up by phone to discuss whether the advice or product was working. ‘Get to the bottom of what is going on, give advice and get the patient to co-create that appointment and plan with you,’ she said.
‘We are used to being the experts and having all the answers, but we need to use a coaching approach, getting the information out of the patient and let them make the decisions,’ she said.
Siobhan now always asks the patient: ‘What messages are you taking away from this appointment?’ She has found that sometimes the answers are unexpected and ‘sometimes you have to go back to co-creating the appointment, rephrasing how you put the advice or information across.’ She suggested clinicians start building that question into their appointments to make sure that patients have completely understood the conversation.
KEY MESSAGES
- Dentine hypersensitivity impacts on quality of life
- Think about the elements of the diagnostic tool and treatment path, and incorporate them in a manageable way into your practice
- Involve the whole team, including the patient, in the management and prevention of DH
- Integrate effective behavioural change tools in the management of DH






